Introduction
Acne vulgaris is a chronic inflammatory skin disorder involving the pilosebaceous unit often resulting from increased sebum production, keratinization, inflammation, and bacterial colonization.1 Additionally, acne is not just a disease that affects adolescents, but adults can be suddenly surprised by an onset of acne and scarring as well. During the COVID-19 pandemic, face mask-induced acne, or ‘‘maskne,’’ has become prevalent among adults. Although acne has been extensively studied, there have been relatively few studies focused on acne scarring—a known sequela of acne vulgaris that can cause permanent disfigurement.2
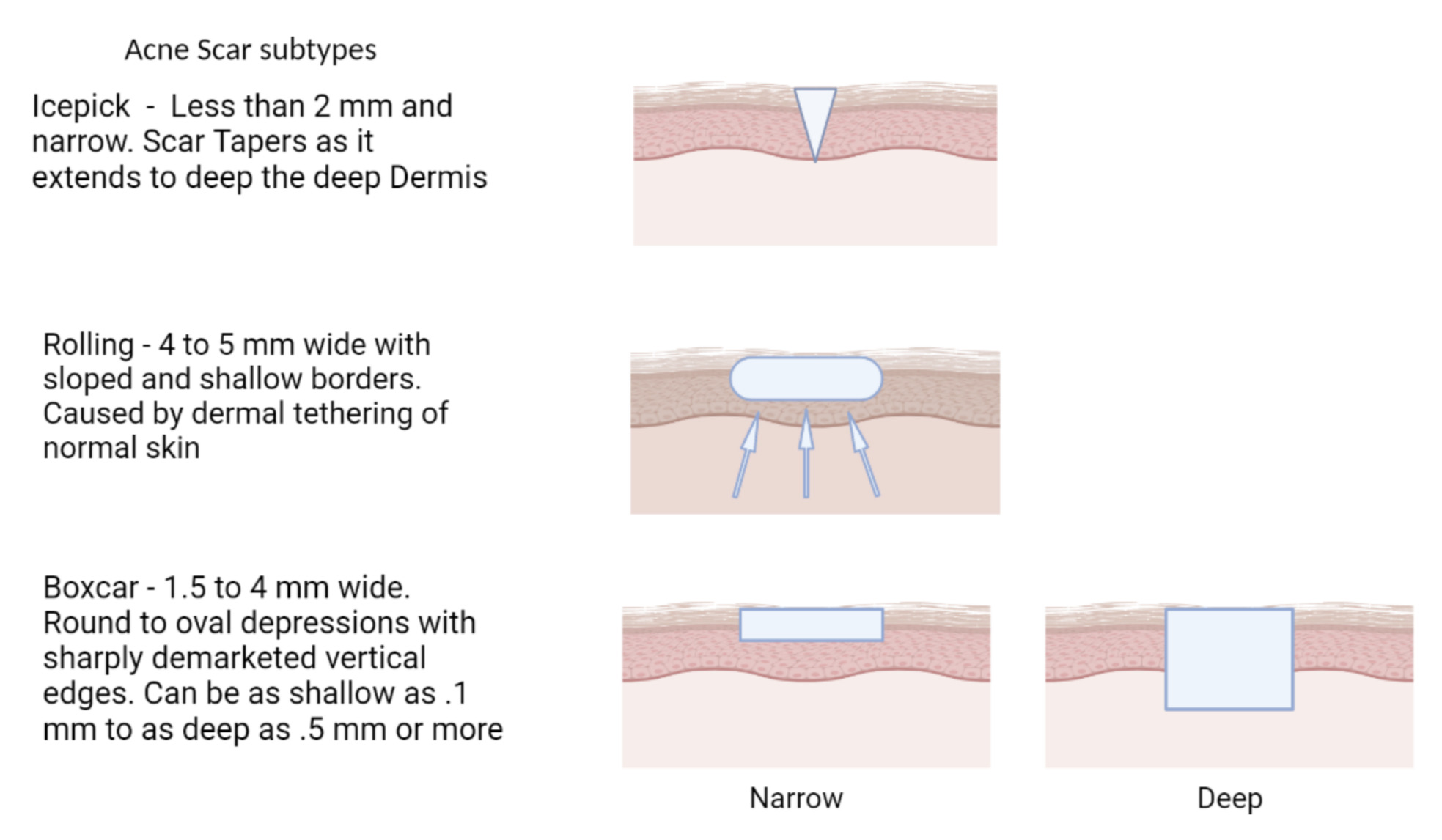
Atrophic scars with a loss of tissue are the most common, presenting 3 times more often than keloids and hypertrophic scars.3 These atrophic scars are classified into ice pick, boxcar, and rolling scars depending on their shape and depth in the skin (Figure 1). There are multiple grading systems for scars that have been used in research settings but generally are not part of routine standard of care in clinical practice. Goodman and Baron have proposed a universally applicable scale based on quantitative features of the scar.4 Hypertrophic and keloid scars are associated with excess collagen deposition and decreased collagen breakdown. While hypertrophic scars respect the boundaries of the original lesion but are elevated, keloid scars grow beyond the original lesion and are characterized by thick bundles of hyalinized acellular collagen.3 These scars often disproportionately affect darker skinned individuals and predominantly occur on the trunk.
A 2017 study of 1,942 patients demonstrated that 43% had acne scarring and even the individuals with mild acne were at risk for scarring.5 As acne scars generally arise from inflammatory acne lesions that are not adequately treated, effective treatment is thought to prevent the risk of scarring.
Many topical and systemic therapies exist for the treatment of acne vulgaris, but there is a paucity of comparative data regarding their effect on acne scarring.6 While there are a number of conventional treatments for the correction of existing acne scars including laser resurfacing, dermabrasion, and chemical peels, these treatments are often expensive and may entail significant downtime, as well as risks of their own.7 Finding non-invasive procedures and treatments for scarring has proven challenging.
In this review, we will review the scarring outcomes related to some of the most commonly used treatments for acne. Oral isotretinoin remains the most efficacious treatment for acne refractory to topical treatments.8 Topically, other retinoids can be used such as tretinoin or adapalene with milder success in efficacy, though with fewer side effects.9 Both topical and oral antibiotics remain common first-line prescription treatments for moderate to severe inflammatory acne; however, their long term use is often not recommended.10 Finally, many patients will often utilize over-the-counter treatment options, such as benzoyl peroxide and salicylic acid.11,12 In this review, we examine the scarring outcomes observed with these treatments, with the acknowledgment that very few clinical trials have specifically looked at scar prevention or treatment.
Current treatment methods and their outcomes
Due to the aberrant production and degradation of collagen during the healing process, acne often results in scarring. In 80 to 90 percent of cases, there is a net destruction of collagen in the dermis that results in atrophic scars. Less commonly, there is a net gain of collagen that results in hypertrophic or keloid scars.3 Many studies unfortunately do not include information on scarring that remains after the treatment of the primary acne lesions. However, there have been a few that provide insightful glimpses into the outcomes. A 2016 cross-sectional observational study evaluating the association between oral isotretinoin and healing abnormalities conducted a 3-phase study. In phase 1, patients were compared during isotretinoin treatment vs no treatment. They found no significant difference in the prevalence of hypertrophic scars and keloids between these two groups. In phase 2, patients were interviewed about scarring after past isotretinoin treatment. Seven of the 8 patients reported improvement of their scars, while one patient stated a new keloid had developed. The final phase looked at patients who were receiving treatments for their keloids and their history of isotretinoin. Here, some of the patients noted their keloids had coincided with an acne flare up that occurred after beginning isotretinoin.13 From this study, the researchers hypothesized that oral isotretinoin influences wound healing, increasing the risk for hypertrophic scars and keloids. However, the incidence itself for this scarring during or after treatment is still relatively low and the researchers emphasized that this study was a pilot and not as longitudinal as they would like.
Another study explored if adapalene 0.3% gel improved the skin appearance and texture of atrophic acne scars over 24 weeks.14 At week 24, ten of the eighteen subjects (56%) showed improvement of 1 or 2 grade from baseline in their scars. Fifteen of the 18 subjects (83%) reported that their skin texture had improved and lesion accounts decreased for all scar types. However, none of these lesion count changes were found to be statistically significant, falling just short at p = 0.06.14 Despite the lack of quantitative support for the treatment, 88.2% of the study subjects were satisfied with the treatment results and reported that they would use it again. An important limitation to acknowledge of this study was the use of a singular treatment and no comparative treatment or control.
As adapalene was shown to be effective in reducing the severity of scarring, a 48-week two-part study was conducted to test a combination of adapalene 0.3% and benzoyl peroxide 2.5% gel (A0.3/BPO2.5). In this study, 45 subjects applied A0.3/BPO2.5 to acne lesions and scars on half of the face for 24 weeks and full face for 24 weeks. The first 24 weeks provided a comparative intra-individual comparison (right half face vs left half face) by applying A0.3/BPO2.5 to only half of each participant’s face. During the initial stage of the study they saw a 21.7% decrease in scarring at 24 weeks and a 26.9% decrease in 48 weeks.15 This demonstrated that topical acne treatment methods used to treat lesions, may be useful for post-acne scarring as well. Additionally, the researchers emphasized the long-term nature of their study compared to other treatments and saw an incremental increase in efficacy on scarring over 24 weeks. They stated: “In fact, 3 months may be sufficient to observe resolution of the primary acne lesions, but the remodeling processes occur slowly, and 6 months may be required to induce significant stimulation of the dermal fibroblasts and collagen and clinically observe an effect on scars.”15
Salicylic acid has extensive proven efficacy in OTC acne treatment especially for redness and inflammation. It is also seen to be a useful chemical peeling agent at higher percentages for the treatment of acne scars as well.3 As a beta hydroxy acid, it removes intercellular lipids that are linked to the cornified envelope surrounding keratinized cells.16 20-30% concentrations are often utilized by clinicians, and while generally safe and well-tolerated, patients may develop temporary or even persistent hyperpigmentation or scarring from the treatment. Salicylic acid may be useful in longitudinal treatment for both acne and scarring, but long-term dryness and irritation may be an issue for many patients.17
A 2019 study looked at a novel agent Tranilast [N-(3,4-dimethoxycinnamoyl) anthranilic acid] for the prevention and treatment of acne scars that were concomitantly treated with isotretinoin.18 They treated half of each patient’s face with the tranilast 8% liposomal gel and the other half with a water-based placebo. They found that for the 32 patients that completed the trial, there was a mean Global Aesthetic Improvement Scale score at 5 months that had a significantly lower scarring for the tranilast-treated side. Additionally, all patients in the tranilast group reported greater satisfaction and better general improvement in skin appearance and texture.18
Discussion and Future directions
Past studies on acne treatments and therapies often lacked a comprehensive evaluation of patient satisfaction. A 2021 study developed an Acne Core Outcome Set, which included a satisfaction metric with acne treatment. This study searched PubMed, Medline, Embase, Lilacs, Web of Science, Cochrane Library, Emcare, PsycInfo, and Academic Search premiere in order to determine patient-reported outcome measures. Unfortunately, their review of all these databases only found one singular study that described the treatment satisfaction as a measure. Additionally, this study was found to lack proper measurements and metrics. However, they found 188 studies that reported treatment satisfaction solely as an outcome, but none of them were standardized.19 This demonstrates the substantial need for more longitudinal studies and the need to document patient satisfaction uniformly.
Another important future direction for clinicians and researchers to be mindful of is the necessity of more objective and uniform assessment of acne scarring. Individual clinicians may grade scar severity differently, and current grading scales lack vital criteria in the assessment of scars. Currently, methods of grading mainly include lesion counting; subjective self-assessment, Acne Scar Rating Scale (ASRS), evaluator-based qualitative and quantitative scarring grading systems, Echelle d’Evaluation Clinique des Cicatrices d’acne (ECCA), Global Scale for Acne Scar Severity (SCAR-S), and use imaging modalities. Despite all these tools and scales, currently available scales do not account for scar color, depth, or change over time.20 These new imaging modalities may provide clinicians with quantitative objective measurements of acne scars that will help in determining treatment effectiveness. These new 3D imaging methods have the capability to evaluate changes in the shape of scars before and after treatment quantitatively.21
Until recently, clinicians have mainly relied on physical invasive treatments for acne scarring with less emphasis on potential prevention of scars as a specific outcome. However, there is emerging evidence of new preventative approaches as listed above.15,22 The 0.3% adapalene and 2.5% benzoyl peroxide is not the only recent development. In 2022, two new studies in the topical treatment of acne scars are of interest. DA-5520 is an investigational topical gel that was tested in a study with 36 participants. Four groups were created, laser resurfacing with DA-5520, laser resurfacing without DA-5520, comedone extraction with DA-5520 application, and comedone extraction without DA-5520. Han et al found clinical improvement by the ECCA grading scale when DA-5520 was combined with laser resurfacing or alone without it as well.23 Finally, a 12-week face split study applied Epidermal Growth Factor significantly improved acne and acne scars.24 Acne lesion and scar counts were significantly reduced after 4 weeks, and investigators’ global assessment for acne, scar, and ECCA scar grading scales were significantly decreased after 8 weeks. They also found decreased expression of keratin 16, NF-κB p65, IL-1α, and IL-8, and increased expression of TGF-β1, elastin, and collagen type 1, 3 after treatment.24
These new treatments (Table 1) offer greater insight into patient satisfaction and provide hope for patients suffering from acne vulgaris and the potential for subsequent scarring. Current challenges in acne scar prevention include a lack of open communication between patients and physicians, as well as poor treatment adherence.22 With hope, patients and clinicians can benefit from therapeutics that work towards both goals. This emphasizes the importance of encouraging maintenance therapy, particularly as patients may find it difficult to adhere to their treatment for long periods of time.22 Some patients may be deterred by long term treatments and thus do not initiate conversations about prevention of future scarring. Fortunately, clinicians and researchers are working hard to progress in the understanding of the underlying pathophysiology of acne scarring. Through early evaluation and treatment, the best potential treatment for acne scarring will not be any procedure, but instead prevention.
Funding Sources
No funding sources were secured for this study.
Disclosures
Dr. Lio reports research grants/funding from the National Eczema Association, AOBiome, Regeneron/Sanofi Genzyme, and AbbVie; is on the speaker’s bureau for Regeneron/Sanofi Genzyme, Pfizer, Eli Lilly, LEO, Galderma, and L’Oréal; reports consulting/advisory boards for Almirall, ASLAN Pharmaceuticals, Dermavant, Regeneron/Sanofi Genzyme, Pfizer, LEO Pharmaceuticals, AbbVie, Eli Lilly, Micreos, L’Oreal, Pierre-Fabre, Johnson & Johnson, Level Ex, Unilever, Menlo Therapeutics, Theraplex, IntraDerm, Exeltis, AOBiome, Realm Therapeutics, Altus Labs (stock options), Galderma, Amyris, Bodewell and My-Or Diagnostics.
The other authors report no conflict of interest.